Labour can sometimes need to be induced for medical reasons or because pregnancy has reached 41-42 weeks.
The UK national induction rate is around 33%
Only 4% of women give birth on their due date
58% of women give birth by 40 weeks
74% of women give birth by 41 weeks
82% of women give birth by 42 weeks
Common reasons for induction include:
*Pre-eclampsia
*Diabetes
*Your amniotic fluid has been leaking for more than 24 hours
*Concerns about your placenta
*Going over your due date
*If you have previously experienced a stillborn baby
*Being over 40
Natural ways to encourage labour to start
These methods might work if labour is imminent or if you are in the early stages of labour. They are more likely to help you to relax, which can be beneficial to labour.
- Walking – gravity can apply pressure to your cervix and it can help your baby move into a better position for labour
- Nipple stimulation – to produce oxytocin
- Sex – the prostaglandin hormone in semen can encourage labour and orgasms can create oxytocin to encourage contractions
- Complementary therapies such as reflexology and acupuncture might also help but see a qualified practitioner who is experienced in working with pregnant women.
Membrane Sweep
- This involves an internal examination by your midwife, who will insert a finger just inside the opening of the cervix and sweep it around. The aim of the sweep is to separate the amniotic sac from the cervix, which may create contractions. Your midwife may also attempt to stretch the cervix as well.
- This can only be done if your cervix has started to soften for labour and if your amniotic sac is still intact, so your waters haven’t broken.
- A membrane sweep can be done at home or at the antenatal clinic from the end of the 40th week of your pregnancy. The later in pregnancy it is done, it increases the chances of labour starting within 48 hours.
- It can be uncomfortable – use your breathing to relax
Afterwards: you may experience some cramping, some discharge and some bleeding so get checked out if that gives you a fright. Try to relax and rest, go for a walk and you could also have sex to encourage labour to start.
Prostaglandin
- This will be done in hospital, although some maternity units are now sending women home afterwards.
- Prostaglandin gel or a pessary is placed next to the opening of the cervix. You may also be given propress, a slow release pessary, which is like a tampon. The pessary/gel may be tried 2-3 times in 24 hours. The propess can be in place for up to 24 hours.
- You will need to lie down for a short while afterwards and you may experience pains and cramping. After about an hour you can move about and be mobile so you feel more comfortable, calm and in control.
- You may feel sick and it can cause hyper-stimulation of the womb in some women.
- Labour often starts gradually, similar to natural labour. Labour starts in 50% of cases.
Afterwards: Try to relax and be distracted while you wait for labour to start so take in plenty to do – a book, your tablet, cards, a movie – and go for a wander around.
Balloon Catheter
- Some maternity units offer induction using a Foley Catheter, which is slowly inflated with saline solution. This gradual pressure on the cervix can encourage it to dilate and it can be in place for about 12 hours.
- It can be an uncomfortable procedure for some women but there is a lower risk of hyper-stimulation on the uterus.
- This method can be offered to women who have previously had a caesarean and labour could start within 24 hours.
- Ask if this is an option available to you.
Artificial Rupture of the Membranes (ARM)
- A midwife uses an amnio-hook to break the amniotic sac.
- Labour can start quickly but the effect of ARM can vary a lot.
- If contractions don’t start, an oxytocin drip may be offered.
- ARM can be offered after labour has started if progress is slow.
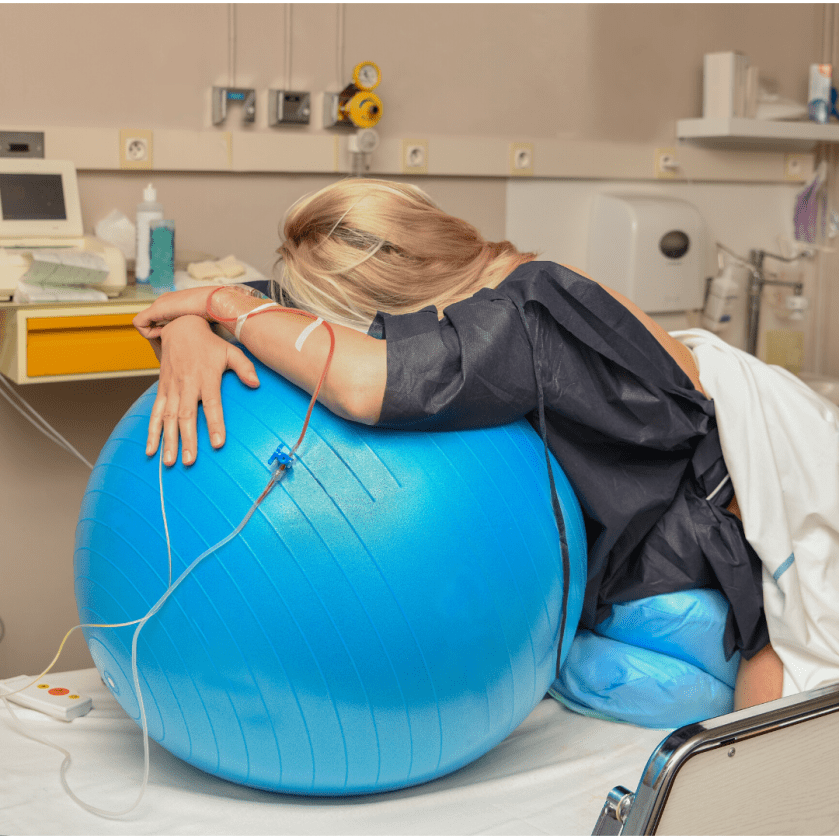
Afterwards: Use your breathing to stay calm and relaxed; get off the bed and move about, sit on your birth ball; rest and keep distracted if your contractions haven’t properly started.
Oxytocin Drip
- Syntocinon, a synthetic form of oxytocin, is given by intravenous drip into the back of the hand or your arm.
- It usually produces strong contractions and the drip can be adjusted to regulate the contractions.
- An epidural can be needed due to the intensity of the contractions, which can have less of a gentle build up than with spontaneous labour.
- Some babies can become distressed due to the intensity of the contractions so your baby will be continuously monitored to make sure they are handling all of the contractions.
After this has been set up: It can be beneficial to get off the bed – make a comfortable nest next to the bed so you can sit, kneel, stand and move as you need to. This will help you to be more comfortable and it will give you more gravity to help your labour flow. You can use a birth ball, a chair, pillows and a bean bag to give you flexibility.
What you might need for your induction
- support
- reassurance
- information
- comfort
- to be listened to if you have any concerns or questions
- encouragement and help to move about and to change position
- birth ball
- pillows
- cushions for the floor
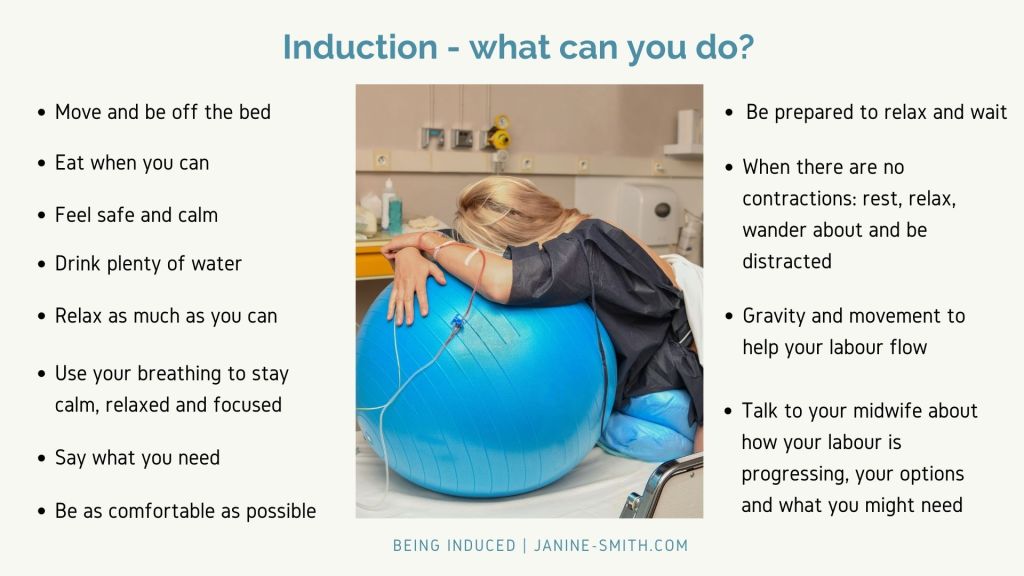
What can you do if you are induced?
- Move about – use gravity and upright positions to stay comfortable, to encourage your baby to stay in a good position and to maximise the space in your pelvis.
- Drink plenty of water, rest when you want to, use your breathing to stay calm and head off any anxiety.
- When you are being induced, it is still important to create your own oxytocin as this creates contractions and helps your labour to progress.
If you feel calm, reassured and safe, this will help you create oxytocin.
- Relax as much as you can – use your breathing to stay calm, to encourage your body to labour. Be aware of any tension in your body and try to let it go
- Take plenty into hospital with you – music, books, games, magazines, your tablet, etc to keep you occupied and distracted while you wait for your contractions to start. Headphones are also a good idea so you can listen to music to help you stay relaxed and calm.
- Get off the bed, move about, use gravity, be comfortable, stay in control.
- Talk to your midwife about your pain management options – what is available for you to use if you need it?

A summary of what you can DO during induction…
- DRINK WATER: so you don’t become dehydrated and tired.
- WEE REGULARLY: go to the loo about every hour, so your bladder is empty and your baby has more room to move into the right position for labour and birth.
- EAT: if you can because you may need energy.
- REST: to conserve your energy.
- BREATHE: know how to control your breathing to stay calm, focused and to handle any panic or anxiety. If you can use your breathing, you can get rid of any tension.
- MOVE: use gravity and different positions to stay comfortable and to work with your contractions.
- SAY WHAT YOU NEED: only you know how you are feeling and what feels right.
- BE WELL PREPARED: read well, invest in good antenatal classes so you have knowledge about your options, what may help and what may not.
- ASK QUESTIONS: so you know what is going on and so you know what your options are.
- FEEL SAFE: have the support you need, be where you want to be.
- LOOK AFTER YOUR BIRTH SPACE: make it comfortable for you so you can move, have the lights dimmed so you can relax, use music/ear plugs to block out any noise.
- DON’T FEAR YOUR CONTRACTIONS: you need them, so don’t battle with them. Try to accept them and work with them in the best way for you – breathing, movement, water, pain relief – but let them have what they need to work: relaxation not tension & gravity not being recumbent.
- DON’T WAIT FOR PERMISSION: do what feels right and talk to your midwife so she can support and guide you.
- BE GUIDED BY YOUR BODY: for movement, comfortable positions, rest, pushing, what feels right and what feels safe.

As you go through this module and the resources, you can make notes, jot down your questions and start to develop your action plan for labour and birth.
And please don’t hesitate to message me below to arrange a conversation with me to talk through your questions.

Welcome To Your Antenatal Course
1. Labour
2. Birth
3. Pain Management
4. Labour & Birth Challenges
5. Meeting Your Baby
6. Your New Baby
7. Relax & Breathe Resources